Thanks to neural networks, a new investment cycle is now available to everyone
A new cryptocurrency investment company, CrypTouch, just recently went live for everyone. For a period of time it was available only in a test mode …
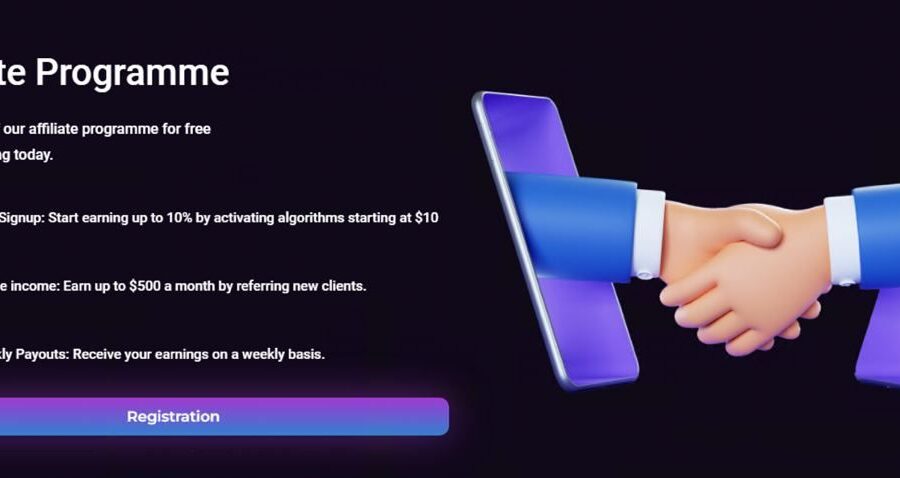
A new cryptocurrency investment company, CrypTouch, just recently went live for everyone. For a period of time it was available only in a test mode …

A quick surge in bitcoin (BTC) on Thursday lifted the price above $44,000 as the benchmark cryptocurrency extended its rally supported by anticipation for a …

BRIANNA Ghey's tragic final hours were captured in haunting CCTV as she left home for the last time to meet her killers. The 16-year-old was …

The United States has announced that alongside American astronauts, it plans to land an international astronaut on the surface of the Moon by the end …

CCData, a global leader in digital asset data and an FCA-authorised benchmark administrator, has released the December 2023 edition of the “Stablecoins & CBDCs” report. …

Donald Tusk, the former European Council president who is now Poland’s Prime Minister, has been accused of “the destruction of democracy” after seizing control of …

The UK faces a deep freeze and significant snow in the days between Christmas and New Year, according to advanced weather maps Although the white …

Keir Starmer warns of ‘real and constant’ Russian threat to the UK as Labour leader seeks to burnish his pre-election defence credentials with Christmas visit to …

Pheasant-hurling driver who threw a dead bird at a married couple in bizarre incident is ordered to pay more than £1,000 George Harker, 20, left …

Proposed EU travel regulations, set to take effect next autumn, include mandatory fingerprint and photo ID checks, raising concerns about potential disruptions and longer wait …